Many men suffer from chronic prostatitis, but attribute the symptoms to other diseases or waste time on ineffective treatment. From our article you will learn comprehensive information about this male problem: causes, exact symptoms and methods of diagnosis, various methods of treatment.
Despite all the successes of modern medicine, diagnosing such a disease as chronic prostatitis causes certain difficulties. This negatively affects the effectiveness of his treatment.
What is chronic prostatitis
In ICD-10 (International Classification of Diseases, 10th revision) there is no such disease as "chronic prostatitis". Also, there is no single, generally accepted characteristic of this pathology. In urological practice, it is customary to use the classification developed by AHI (American Institute of Health). It defines the categories of prostate diseases. Those that can be described as "chronic" include:
- chronic bacterial prostatitis;
- chronic abacterial prostatitis.
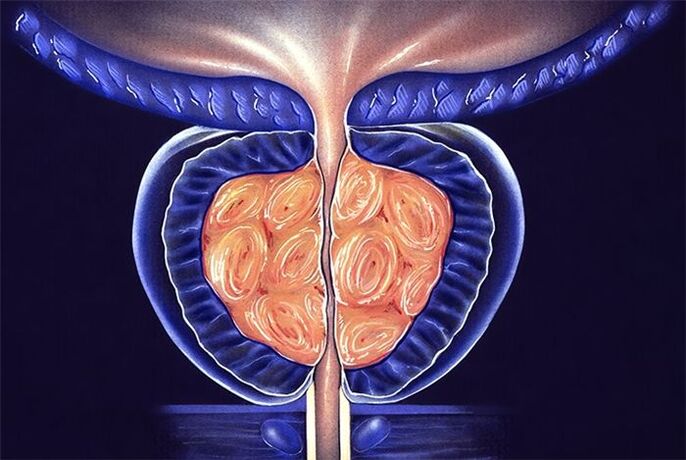
To make these diagnoses, the following symptoms are necessary: prolonged (at least 3 months) pain in the perineum. Thus, chronic prostatitis can be called a prolonged inflammatory process that leads to changes in the structure of the prostate gland and its dysfunction. But other prostate diseases also lead to such sad results. Therefore, the diagnosis of chronic prostatitis is difficult.
Epidemiology
Prostatitis is one of the most common diseases in men. It has a significant impact on work and family relationships. The patients' quality of life is reduced to the same extent as in people who have had a heart attack or suffer from angina pectoris.
According to various sources, every 3rd or 4th man is diagnosed with prostatitis. And most often this is not an initial or acute stage of the disease, but an already formed and long-running process - chronic.
Not so long ago, it was believed that this pathology is inherent mainly in elderly men. But the statistics refute this thesis. Today it is known that chronic prostatitis is a disease of men of childbearing age who lead a sexual life.
More than 30% of patients turn to a specialist with complaints characteristic of the chronic form of prostatitis. Often, during the visit to the doctor, the disease is complicated by concomitant pathologies: erectile dysfunction, vesiculitis, primary or secondary infertility, epididymitis.
Causes of chronic prostatitis
The causes of chronic prostatitis are very different. From all the variety of negative factors affecting human health, it is difficult to isolate exactly those that provoke the development of the disease. Often it is a complex of situations and circumstances that accompany a person's life.
The main causes of chronic abacterial prostatitis are the following:
- dysrhythmia (irregularity) of intercourse;
- hypodynamia, characteristic of overweight people;
- prolonged stressful conditions;
- the predominance of foods rich in fat in the diet;
- negative impact on the body in hazardous productions.
Chronic bacterial prostatitis is the result of incompletely cured bacterial prostatitis. Or the man ignored the ailments and did not seek help from a urologist. Therefore, no treatment was administered.
Chronic prostatitis of abacterial type develops due to exposure to infectious agents against the background of a decrease in immunity. As a rule, diseases of the endocrine system are diagnosed in such patients.
Factors provoking the development of chronic bacterial prostatitis are:
- surgical operations on the prostate (if antibiotic therapy was not carried out before the operation);
- refusal to use contraceptives;
- lack of habit of keeping the body clean.
Symptoms of chronic prostatitis
Today there is a lot of fiction about chronic prostatitis. For this reason, all temporary disorders of sexual function are attributed to this disease. You can often hear the opinion that a decrease in sexual desire and erectile dysfunction are due to prostatitis, and if a person is old, then chronic prostatitis.
This is not true, because sexual dysfunction has many other causes, and the main symptom of chronic prostatitis is pain. All other signs can be considered collateral and indirect.
Chronic prostatitis is often confused with pelvic pain syndrome, as the symptoms of these diseases are largely similar. This is due to the formation of myofascial trigger zones near the prostate, which appear as a result of injuries and surgical interventions. Pain in these areas can be taken as a symptom of prostate inflammation.
When diagnosing the disease, complaints of pain and discomfort in the perineum and pelvis, lasting at least 3 months, come to the fore. The pain is localized near the prostate, radiating to the sacrum, rectum, scrotum. With prolonged exposure to negative factors (carrying heavy loads, excessive physical activity, a long time "on your feet"), the pain intensifies.
A characteristic symptom of the disease is premature ejaculation. Patients have reduced sexual desire, erectile dysfunction. These symptoms are also characteristic of other diseases of the urogenital area. Therefore, it cannot be said that they are hallmarks of chronic prostate disease.
An important symptom is the fading of orgasm. If the patient begins to notice that the sharpness of sensations during ejaculation has disappeared, this is an occasion to pay more attention to his health and a signal to visit a urologist.
The structure of the inflamed prostate becomes denser, the pressure on the urethra increases, and the quality of urination deteriorates. Patients with chronic prostatitis note a frequent urge to urinate at night. The process of passing urine is accompanied by a burning sensation, pain, pain. Urinary incontinence is common.
Signs of chronic prostatitis can be expressed in whole or in part. Much depends on the patient's state of health, the presence or absence of other diseases. Chronic prostatitis is characterized by an undulating course, with increasing and decreasing symptoms. In this disease, the inflammatory process is not acute.
Diagnosis of chronic prostatitis
In the presence of severe symptoms, the diagnosis of chronic prostatitis is easy. But this disease is often asymptomatic, which complicates its detection. For diagnostic purposes, a whole range of research is conducted.
The Association of Urologists has developed questionnaires, thanks to which it is possible to identify asymptomatic chronic prostatitis. The questions are formulated in such a way that the subjective feelings of the patient can be established. Not every man is able to give a correct assessment of his erectile function, the quality of orgasm and other details of sexual life. The questionnaires filled out by the patients provide the specialist with the necessary information to make the diagnosis. In urological practice, the NIH-CPS scale is most often used.
To distinguish chronic prostatitis from other diseases, a neurological examination is performed. In the list of diagnostic methods used, the determination of the patient's immunity status.
Laboratory research methods
If you suspect chronic prostatitis, first find out what its nature is: bacterial or abacterial. In the first case, it is necessary to determine the pathogen or pathogens in order to find out which drugs they are sensitive to. For this, laboratory tests of urine and prostatic secretion are carried out.
If, after a 10-day period after the DRE, the PSA test showed an excess of the prostate-specific antigen level of 4. 0 ng / ml, this is a reason to refer the patient to a biopsy to rule out an oncological process.
The following research methods are recommended:
- scraping from the urethra;
- general and biochemical analysis of urine;
- LHC culture of prostate secretion.
Instrumental research methods
TRUS (transrectal ultrasound) is performed using equipment equipped with an instrument that is inserted into the patient's rectum. If a hypoechoic area with an irregular shape is found, there is every reason to suspect a malignant neoplasm. In chronic prostatitis, scars, thickening of the structure of the glandular tissue, changes in the seminal vesicles can be observed.
UDI is the main method of functional diagnostics. It allows you to understand the nature of urination, signs of urine stagnation, its composition. The examination includes several tests: uroflowmetry, cystometry, measurement of residual urine volume, assessment of bladder pressure and urine outflow rate.
Tomography (computed or magnetic resonance) is necessary to exclude benign and malignant neoplasms. These research methods are very informative and help to assess the condition of the prostate tissues.
Treatment of chronic prostatitis
Treatment of chronic prostatitis requires an integrated approach. One dose of medicine is not enough. Physiotherapy procedures, therapeutic exercises are necessary. In general, chronic prostatitis is difficult to treat, requiring a radical revision of the lifestyle, a change in habits, and in some cases a change of work. Urologists insist that only a set of measures will help to completely get rid of this disease or ensure long-term remission.
Regardless of whether the disease is bacterial or non-bacterial in nature, congestion in the prostate plays a major role in its formation. The viscous secretion deposited in the ducts of the gland is a favorable environment for the development of pathogenic and opportunistic microorganisms. That is why the main focus should be on removing stagnation.
The problem is solved by changing the lifestyle and including physical therapy exercises in the daily schedule.
Complexes of exercises have been developed that are suitable for different life situations:
- for those men who are forced to sit most of the time (drivers, office workers, managers);
- for overweight people;
- for those who don't have time to exercise.
Thinking about how to treat chronic prostatitis, you should decide to seriously reconsider your attitude to your health.
Treatment of acute prostatitis
Acute prostatitis requires bed rest, a special salt-free diet and sexual rest.
Course treatment methods:
- The most effective in the treatment of prostatitis is etiotropic therapy. If the basis of prostatitis is an infection, a course of antimicrobial agents is a priority, which relieves the manifestations of inflammation.
- The pain syndrome is relieved with analgesics, antispasmodics, rectal suppositories, microclysters with warm solutions of painkillers. NSAIDs may be used.
- Immunostimulants, immunomodulators, enzymes, vitamin complexes, a combination of trace elements have proven their effectiveness.
- Physiotherapy methods are possible only in the subacute stage of the disease. They improve microcirculation, increase immunity: UHF, microwave oven, electrophoresis, laser, magnetotherapy.
- Massage is another effective method of affecting the prostate. Opens the channels, normalizes the blood circulation of the scrotum, small pelvis.
- Acute retention of renal filtrate can be corrected by catheterization, trocar cystostomy.
- The purulent process involves surgical intervention.
- Consultations with a psychologist.
Treatment of chronic prostatitis
With prolonged (at least one month) exposure to the prostate, there is no 100% guarantee of cure. Priority of herbal preparations, immunocorrection, change of household habits:
- Phytopreparations are widely used in urological practice. They are able to accumulate at the site of the most active pathological process, protect cells from oxidation, remove free radicals and prevent the growth of glandular tissue.
- Antibacterial therapy is selected individually, based on the sensitivity of microbes to drugs.
- Medicines to increase immunity not only help to cope with prostatitis, but also correct the negative effect of antibiotics that disrupt the function of the immune system.
- The pain syndrome is stopped by the appointment of alpha-blockers, muscle relaxants.
- Prostate massage allows you to mechanically remove the "extra" secretion of the gland through the urethra, improve blood circulation and minimize congestion.
- Physiotherapy: laser, magnet, ultrasound, iontophoresis, sitz warm baths or herbal micro-enemas.
- In severe cases, intravenous fluids with diuretics are indicated. This stimulates the copious excretion of urine, prevents the symptoms of intoxication, the development of ascending cystitis, pyelonephritis.
- For constipation, laxatives of plant origin are used.
- The urologist, the psychologist, together with the patient, develops an individual long-term program for daily routine, necessary rest, diet, dosed physical activity and sexual activity.
- In case of resistance of the chronic process to the ongoing therapy, blocking the outflow of urine, surgical intervention is prescribed: removal of all affected tissues (transurethral resection of the prostate) or complete removal of the gland with surrounding tissues (prostatectomy). It is practiced in exceptional cases, filled with impotence, urinary incontinence. Young people do not undergo surgery, as it can cause infertility.
Recommendations for outpatient treatment
The patient should avoid situations in which injuries to the pelvic organs may occur.
It is necessary to exclude any load on the prostate: do not ride a bicycle, do not do strength exercises, do not carry heavy loads.
If the work is sedentary, every 2-3 hours it is necessary to warm up, do squats, leg swings, running in place.
It is necessary to try to normalize sex life, which is extremely important to eliminate the stagnation of secretions in the prostate.
It is recommended to limit to the minimum doses or completely eliminate the use of alcohol.
Drug treatment
Chronic prostatitis is mainly treated on an outpatient basis. If the pathological process continues and it is not possible to achieve remission with this method, hospitalization is recommended. In a hospital, under the supervision of medical personnel, there are many more opportunities to observe the regime and monitor changes in the patient's condition.
Chronic prostatitis in men develops against the background of endocrine disorders. In this regard, 5-alpha reductase inhibitors and alpha 1-blockers are recommended. They contribute to normalizing hormonal levels and eliminating the symptoms of pathology. For these purposes, drugs such as finasteride and terazosin are prescribed.
The integrated approach includes taking drugs such as:
Methods of treatment of bacterial chronic prostatitis
Bacterial chronic prostatitis is treated with antibiotics. The most effective drug for a particular patient is determined with the help of a preliminary laboratory study of prostate secretion.
There is no universal drug to suppress and destroy the pathogenic microflora. What works for one patient may not work for another. For this reason, there are many negative reviews of advertised drugs for the treatment of chronic prostatitis.
The recommended drugs for antibacterial therapy are fluoroquinolones. Most bacteria are sensitive to them.
Antibiotics may also be included in the treatment plan for patients with abacterial prostatitis. Such therapy is carried out for preventive purposes. According to the indications, treatment with penicillin preparations is associated.
After completion of antibiotic therapy, treatment with hormonal drugs begins.
In case of intraprostatic reflux, it is necessary to take α-blockers.
Pain relievers are effective in relieving pain.
Treatment with herbal preparations
Many people doubt whether chronic prostatitis can be cured with herbal medicines. The answer to this question was obtained from the many years of use of these means to improve health in urological practice.
Today, the following treatment complexes are recommended:
All these drugs have a beneficial effect on the work of the male genitourinary system. Effective treatment of chronic prostatitis is possible if urination function is normalized. The components that make up herbal medicines perform this task. They help to reduce the frequency of urges, eliminate the syndrome of a slow stream.
Patients with chronic prostatitis are recommended phytocollections that include pumpkin extract or pumpkin seeds. The latter have a unique chemical composition and act simultaneously in three directions:
- normalizes metabolism;
- strengthening the walls of blood vessels;
- activation of blood circulation in the pelvic organs.
Taking herbal medicines cannot be considered as the main method of treatment. These remedies are considered adjunctive drug therapy.
Non-drug treatment
Non-drug methods of therapy allow you to act directly on the prostate, increase the concentration of drugs in its tissues, help eliminate congestion.
The following methods are used for these purposes: rectal ultrasound exposure;
Microwave hyperthermia is performed using a rectal probe that is inserted into the patient's anus. On the device, you can set the temperature required for a certain type of exposure. To increase the concentration of the drug in the prostate, heating to 38-40°C is required. To achieve an antibacterial effect - 40-45 ° C.
Today, non-drug treatment focuses on laser therapy. The possibilities of this technique are wide. Under the influence of a laser in the prostate gland, the following processes take place:
- activation of redox reactions;
- improves blood microcirculation;
- new capillaries are formed;
- pathogenic microflora is suppressed;
- the process of cell division is activated, which contributes to tissue regeneration.
In the period of research on the effects of laser therapy in patients with prostatitis, a side effect was noted, but positive for the purposes of treatment. In those who have completed the course, potency increases, erectile dysfunction is eliminated and vitality is restored. To achieve this result, it is necessary to use a beam of a certain wavelength. Generally, low-intensity laser radiation is used to treat chronic prostatitis.
Patients can, on their own initiative, undergo a course of laser therapy if it is not prescribed by the attending physician.
Surgical treatment of chronic prostatitis
Chronic prostatitis does not pose a threat to the patient's life, but it can significantly reduce its quality. The most serious complication of this disease is the formation of stones in the tissues of the gland. To get rid of prostatitis, transurethral resection is used.
Surgery is performed under TRUS guidance.
If complications such as prostatic sclerosis occur, transurethral electrosurgery is performed. If sclerosis of the bladder neck is observed in combination with this pathology, a partial resection of the prostate is performed.
In case of obstruction of the seminal and excretory ducts, endoscopic operations are indicated to remove the disorders of secretion permeability. For this purpose, an incision is made on the seminal vesicles and excretory ducts. In the case of an abscess, complete removal of the gland is possible.
Exercises for the treatment of chronic prostatitis
There are a number of exercises that are effective in stimulating the prostate, which helps clear congestion. This complex was developed for patients with hip joint problems. Practice shows that these exercises are useful for those diagnosed with prostatitis. Classes can be held at a convenient time, the complex will take no more than 15 minutes to complete.
Exercise #1
- Lie on a gymnastic mat, stretch both arms up.
- They bend their knees and pull them towards themselves, simultaneously spreading them in different directions.
- Lift the pelvis as far as they can.
- Repeat 10-12 times.
Exercise #2
- Standing on the mat, do deep squats.
- Repeat 10-12 times.
Exercise #3
- Lie on your stomach.
- Lift one leg up, then the other.
- Repeat 10-12 times.
When performing this set of exercises, all movements should be smooth. This is the main condition for obtaining a high therapeutic effect.
Treatment prognosis
Few men manage to completely cure chronic prostatitis. Prostatitis often goes into a stage of long-term remission. But when conditions arise to activate the pathology, a relapse occurs. The exacerbation begins with the appearance of pain in the prostate. Often they are accompanied by urination disorders. At the first symptoms of a relapse, you should seek help from a specialist.
Patients are advised to visit a urologist regularly, at least once every six months. With the same frequency, they conduct tests on the condition of the prostate, do an analysis for PSA. With systematic monitoring of the state of the gland, it is possible to promptly identify the processes that provoke a relapse of the disease. But even with a long remission, there is no guarantee that it will not be violated.
The patient must follow the recommendations to prevent exacerbation of the disease. It is recommended to balance the diet by excluding fatty and spicy foods from it. The intake of phytopreparations and traditional medicine must be agreed with the attending physician. With this approach, you can minimize the risk of exacerbation of chronic prostatitis.
Prevention
In order to prevent the appearance of an unpleasant disease for men, it is necessary to eliminate the provoking factors and follow simple rules:
- Lead a healthy lifestyle, give up bad habits.
- Don't get cold.
- Drink at least 1. 5-2 liters of water a day.
- Strengthening immunity, walking a lot, hardening.
- Engage in physical education and sports, visit fitness clubs.
- Avoid stressful situations.
- Practice a regular sex life with a regular partner.































